School Shoes
Choosing the right shoes for your child
The end of the year is nearing and so is the time to start buying next year’s school supplies. This includes our children’s school shoes. But which is the best option for your child? And why is it so important to choose the correct pair?
Choosing the correct footwear can have amazing effects on your child’s walking and foot position long term. From a Podiatry perspective we can see the benefits first-hand in the clinic every day. Conversely choosing the incorrect pair can result in changes in your child’s walking patterns (in-toeing), increasing fatigue and irritation, causing pain to their feet and/or legs and can cause the footwear to wear out very quickly.
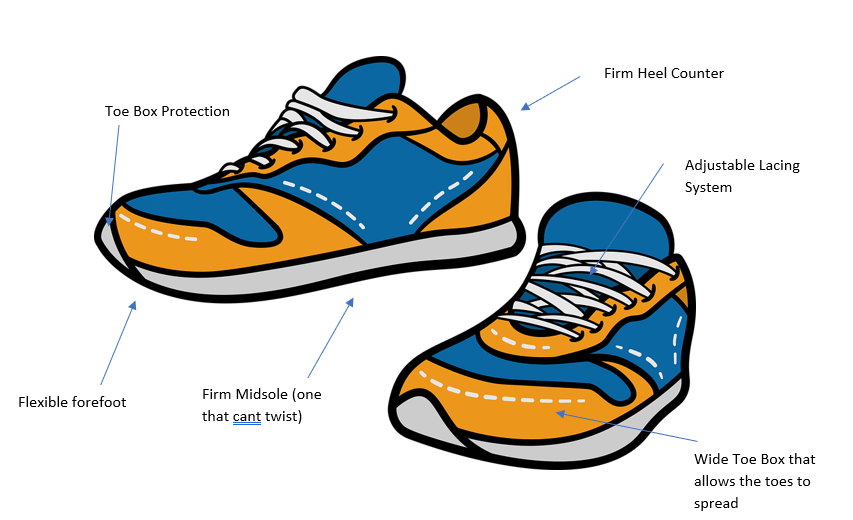
Here are some key features that we look for in a good pair of school shoes:
- Toe box protection
- Flexible forefoot
- Firm midsole (one that can't twist)
- Firm heel counter
- Adjustable lacing system
- Wide toe box that allows toes to spread
Other features that can also be beneficial include:
- Velcro straps
- Full grain leather upper
- 1cm room for growth between your child’s longest toe and the end of the shoe
- Ensuring the type of shoe you are getting your child is appropriate for their activities (i.e. do they need a formal shoe? A running shoe? A cross training shoe?
- Lightweight
If this is something you would like our Podiatrists to help with or you are still confused on what to buy for your kids book online or give your local Better Movement Clinic a call.